
The team also found that on average, women lost a greater percent of their body weight than men. “We found that individuals with more severe obesity lost a greater percent of their body weight than those with less severe obesity,” says Jastreboff. They found that participants who had a baseline BMI greater than or equal to 35 lost more weight than participants with a lower BMI. The team studied baseline body mass index (BMI) and sex.
#NEW ENGLAND JOURNAL OF MEDICINE COVID TRIAL#
The trial also explored how baseline characteristics of patients may predict how well they will respond to the medication. Food and Drug Administration (FDA) has deemed the 5% threshold to be clinically significant-in other words, this degree of weight reduction is linked to metabolic and other health benefits. Furthermore, all participants receiving an 8 mg or 12 mg dose met their weight reduction target of greater than or equal to 5% of body weight. Participants who received the highest dose of retatrutide on average lost nearly a quarter of their baseline body weight (24.2%) over the 11 months of the trial-on average, 58 pounds. Of those in the experimental group, participants received varying dosages ranging from 1 mg to 12 mg. The trial enrolled 338 patients who were randomized to receive a weekly injection of retatrutide or a placebo for 48 weeks. The recent phase 2 clinical trial led by Jastreboff and published in the New England Journal of Medicine on June 26 evaluated the efficacy and safety of this molecule. Retatrutide is a novel triple-hormone-receptor agonist that targets three nutrient-stimulated hormone receptors-glucose-dependent insulinotropic polypeptide (GIP), glucagon-like peptide 1 (GLP-1), and glucagon (GCG). Retatrutide Is Highly Effective in Treating Obesity The goal of the new nutrient-stimulated hormone-based medications, such as semaglutide and tirzepatide, that Jastreboff and colleagues are evaluating is to safely and effectively treat obesity by reregulating this system.
#NEW ENGLAND JOURNAL OF MEDICINE COVID DRIVERS#
However, drivers of obesity-including highly processed foods, increased stress, lack of physical activity, and decreased sleep-can pathologically alter this system and make it extremely difficult to lose weight. The body has evolved a beautiful, intricate system in which hormones send signals to the brain about the body’s energy state. Because obesity is associated with as many as 200 weight-related diseases, developing highly effective and safe interventions that address the underlying causes of disease is critical. And by 2035, researchers estimate that the disease will affect nearly a quarter of the world’s population. Obesity is a chronic neurometabolic disease that impacts nearly half of Americans. “We are truly transforming the way we can care for our patients with obesity now and going forward with these emerging new pharmacotherapeutics.”

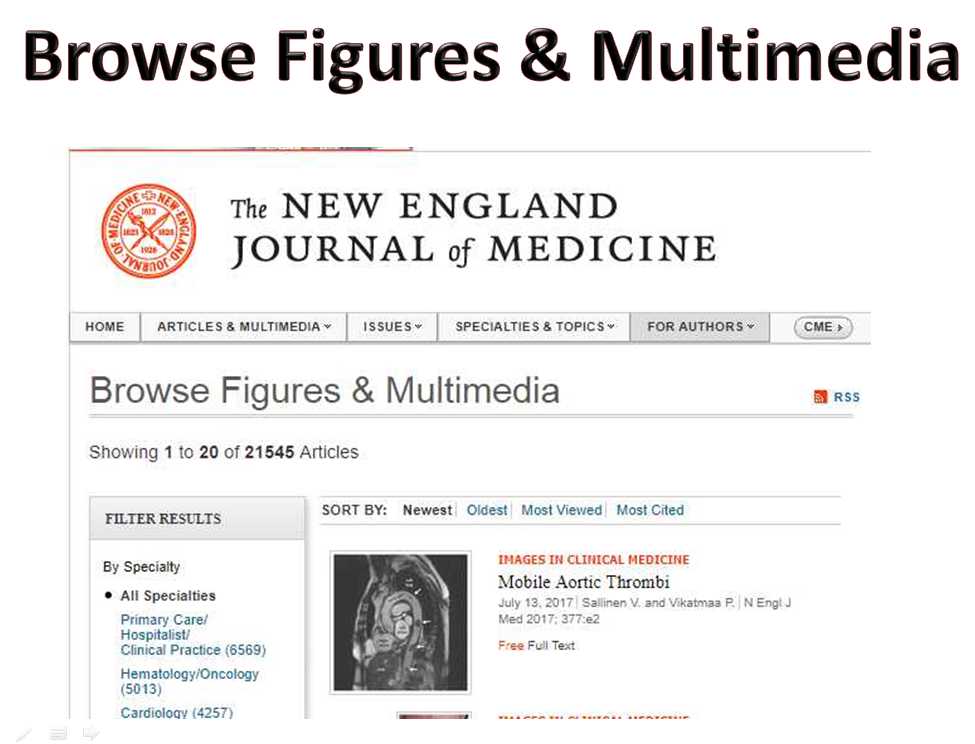
“It’s an exciting time to lead research in the rapidly evolving landscape of anti-obesity pharmacotherapeutics,” says Ania Jastreboff, MD, PhD, associate professor of medicine (endocrinology) and of pediatrics (pediatric endocrinology), director of the Yale Obesity Research Center (Y-Weight) and co-director of the Yale Center for Weight Management, and a leader in studying this new class of therapeutics. While not yet FDA-approved for chronic weight management, they show promise to eventually outshine the current drugs dominating the market. Among the drugs researchers are evaluating are retatrutide and tirzepatide (the latter, FDA-approved for type 2 diabetes), which are weekly injectable medications that clinical trials are showing to be highly effective in treating obesity and type 2 diabetes. Now, numerous clinical trials are exploring new pharmacotherapies that target the mechanisms underlying the disease. The United States and countries around the world are facing a skyrocketing obesity epidemic, but until recently, clinicians had few effective therapies to offer patients. We are truly transforming the way we can care for our patients with obesity now and going forward with these emerging new pharmacotherapeutics. More novel medications are coming down the pipeline that will further revolutionize obesity medicine, with much of the cutting-edge work being led at Yale with three simultaneous publications in the New England Journal of Medicine and Lancet in June. The unprecedented drug offers a safe and effective option for patients that addresses the root of obesity. Semaglutide, also known by its brand names Ozempic and Wegovy, marks a new era in anti-obesity therapeutics.


 0 kommentar(er)
0 kommentar(er)
